In a recent study published in Nature Communications, researchers used ribonucleic acid (RNA) sequence data to understand the association between inflammatory cytokines and poor outcomes of pediatric Acute Myeloid Leukemia (pAML).
Background
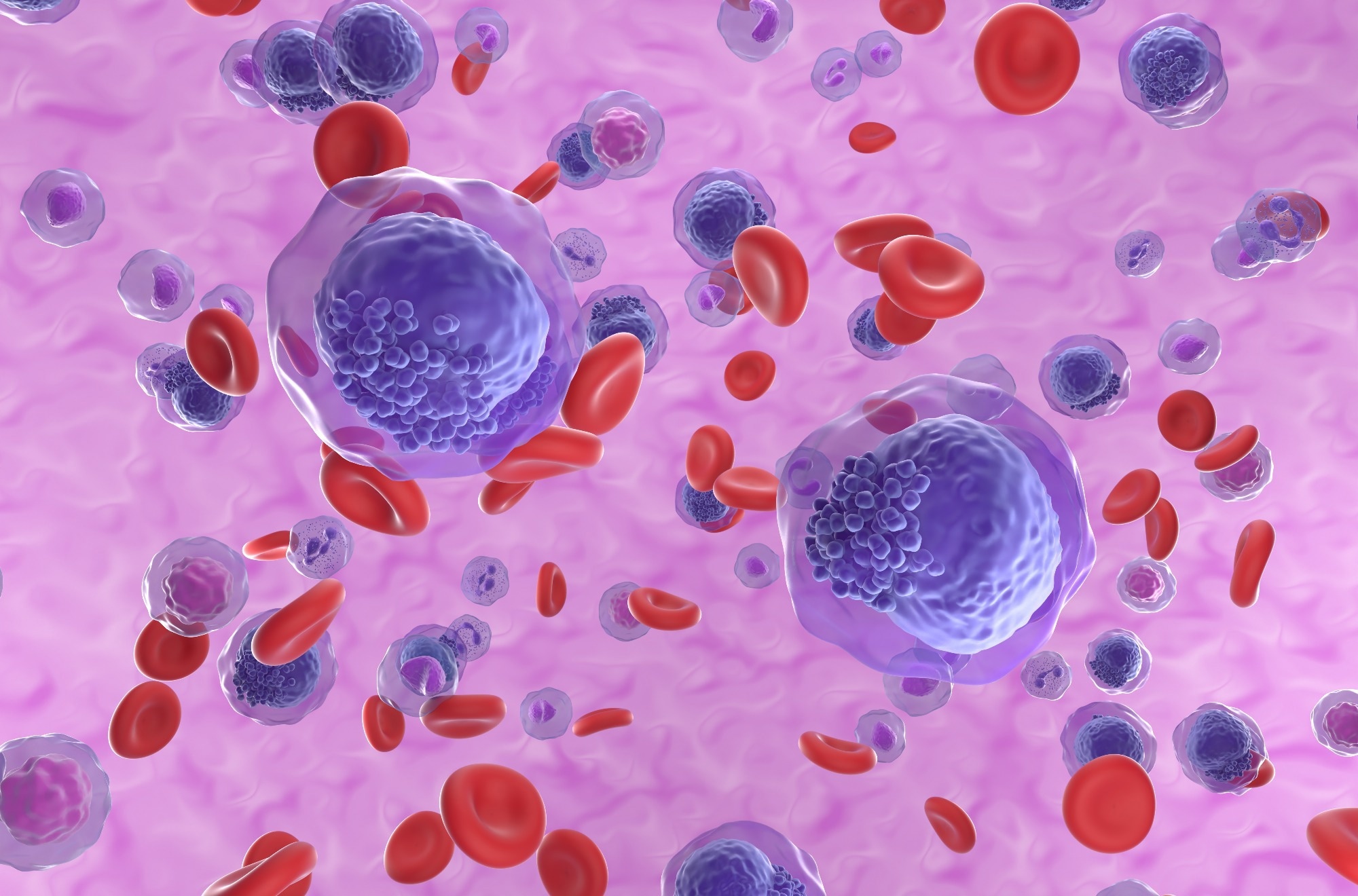
Pediatric acute myeloid leukemia is a heterogeneous disease with various subtypes based on genetic, clinical, transcriptional, and epigenomic factors. The development of therapies that target the clinical outcomes of each of these subtypes is economically challenging. Targeting dysregulated pathways common across various pAML subtypes with poor outcomes can help make treatment methods more cost-effective.
Pro-inflammatory cytokine signaling pathways such as those of interleukin (IL)-6 are linked to various cancers, with IL-6 and IL-3 in synergy increasing hematopoietic stem cell proliferation and poor outcomes of adult and pediatric AML being associated with high levels of IL-6 in the bone marrow. In adult AML, IL-6 also upregulates the Janus kinase (JAK)-signal transducer and activator of transcription (STAT) signaling pathway in stem cells and blood cell progenitors.
Treatment with JAK/STAT pathway inhibitors or antibodies that neutralize IL-6 has shown promise in adult AML cases. Understanding the role of IL-6 signaling in pAML and the association of IL-6 with the pAML subtypes with poor clinical outcomes can further the development of broad targeted therapies for various subtypes.
About the study
In the present study, the researchers collected bone marrow samples from approximately 1500 patients enrolled in the Children’s Oncology Group who were diagnosed with pAML. Total RNA was extracted, and bulk RNA sequence data were compared with those extracted from healthy controls with normal bone marrow.
The researchers then conducted gene set enrichment analyses to understand the signaling pathways associated with high IL-6 levels in certain patient groups. The findings were verified using previously published bone marrow RNA sequence data from an independent cohort. The immunological, genetic, demographic, and transcriptomic profiles of patients expressing high levels of IL-6 and IL-6 receptors were also analyzed.
Bone marrow cells from pAML patients expressing high levels of IL-6 and IL-6 receptors were cultured in human bone marrow stromal cells (HS-5 cells), which replicate the patterns of bone marrow stromal cell expression such as secretion of IL-6, IL-1β, the ligand for receptor-type protein-tyrosine kinase (KIT), and macrophage/granulocyte colony-stimulating factors M-CSF, G-CSF, and GM-CSF.
The bone marrow cells were cultured in the presence and absence of Ruxolitinub, which inhibits JAK1/2 and signaling by various interferons (IFN), tumor necrosis factor-alpha (TNF-α), IL-6, and GM-CSF. The cytokine signaling mediators were analyzed using cytometry by time of flight (CyTOF).
Furthermore, genes expressed differentially in the bone marrow of pAML patients with high IL-6 and low IL-6, as well as in the normal bone marrow of healthy controls, were analyzed using pairwise differential expression analysis.
Results
The results reported that more than 20% of pAML patients had high levels of IL-6 and higher inflammatory cytokine signaling activity, such as TNF-α, IFNα and IFNβ, and IL-1. These high levels of inflammatory cytokines and signaling activity were also associated with poor outcomes, such as a lower probability of event-free and overall survival for two years.
Adjusting for age and cytogenic subtypes within the high IL-6 group did not improve the two and five-year overall survival, indicating that poor outcomes and response to treatment were mediated by factors not related to cytogenetics and age. Furthermore, the CyTOF analysis indicated that distinct genomic subtypes of pAML having high IL-6 and IL-6 receptor levels have common pathways of receptor-mediated inflammatory signaling. Other studies in adult AML patients also found similar patterns of upregulated GM-CSF, IL-6, and IL-1.
Targeted sequencing identified five recurrent regions of somatic mutations, including various translocations and rearrangements that activated common STAT-mediated signal transduction and phosphoinositide-3-kinase–protein (PI3K) signaling pathways. The genomic subtypes associated with these somatic mutations also showed activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB).
Irrespective of the genomic subtype, high IL-6, and IL-6 receptor levels were seen to be associated with the activation of the JAK/STAT, NF-κB, extracellular signal-regulated kinase 1/2 (ERK1/2), and PI3K pathways, and the in vitro inhibition of JAK1/2 by Ruxolitinub was shown to downregulate receptor-mediated signaling by inflammatory cytokines.
Conclusions
Overall, the results reported that high IL-6 and IL-6 receptor levels in pAML patients were associated with genetic subtypes based on five somatic mutations. However, irrespective of the subtype, pAML patients with high IL-6 levels had upregulated inflammatory cytokine signaling pathways and activated JAK/STAT, NF-κB, ERK1/2, and PI3K pathways.
Therapies comprising inhibitors of these co-activated pathways might benefit high IL-6 pAML patients by reducing the inflammatory cytokine signaling pathways across genetic subtypes.