Worldwide, respiratory syncytial virus (RSV) causes a significant burden of disease among infants. According to estimates, more than 101,000 children under five die every year. Although more than 97% of RSV-related deaths occur in low and middle-income countries, the RSV healthcare burden is also quite significant in high-income countries.
Passive immunization with palivizumab is available for high-risk groups, including children with bronchopulmonary dysplasia or heart disease and premature infants. However, high morbidity is observed in infants younger than six months, irrespective of the availability of palivizumab. Several passive immunization trials and maternal vaccines are in phase 3 or are submitted for regulatory approval. It is expected that within 1 to 3 years, one or more of these will be approved. They can then be implemented as prevention strategies by governments into their national immunization schedule. Accurate information regarding the healthcare burden of RSV on healthy infants is required to evaluate these prevention strategies’ economic and health benefits.
Most studies intended to determine RSV-associated hospitalization rates in young children were country-specific, involved children with comorbidities, and were partly based on estimates compared to actual numbers. Although birth cohort studies provided an accurate estimation of disease incidence, they were done in a country or center and thus were not generalizable. The EU Commission funded the Respiratory Syncytial virus Consortium in Europe (RESCEU) to obtain data on long-term consequences and incidence of RSV infection among healthy infants that would, in turn, help to prepare for the introduction of RSV immunization.
A new study in The Lancet Respiratory Medicine journal aimed to determine hospitalized and medically-attended RSV-associated respiratory infections in healthy infants across Europe. The study also estimated the incidence of symptomatic RSV infections, the proportion of respiratory infections caused due to RSV, and the incidence of all-cause respiratory infections.
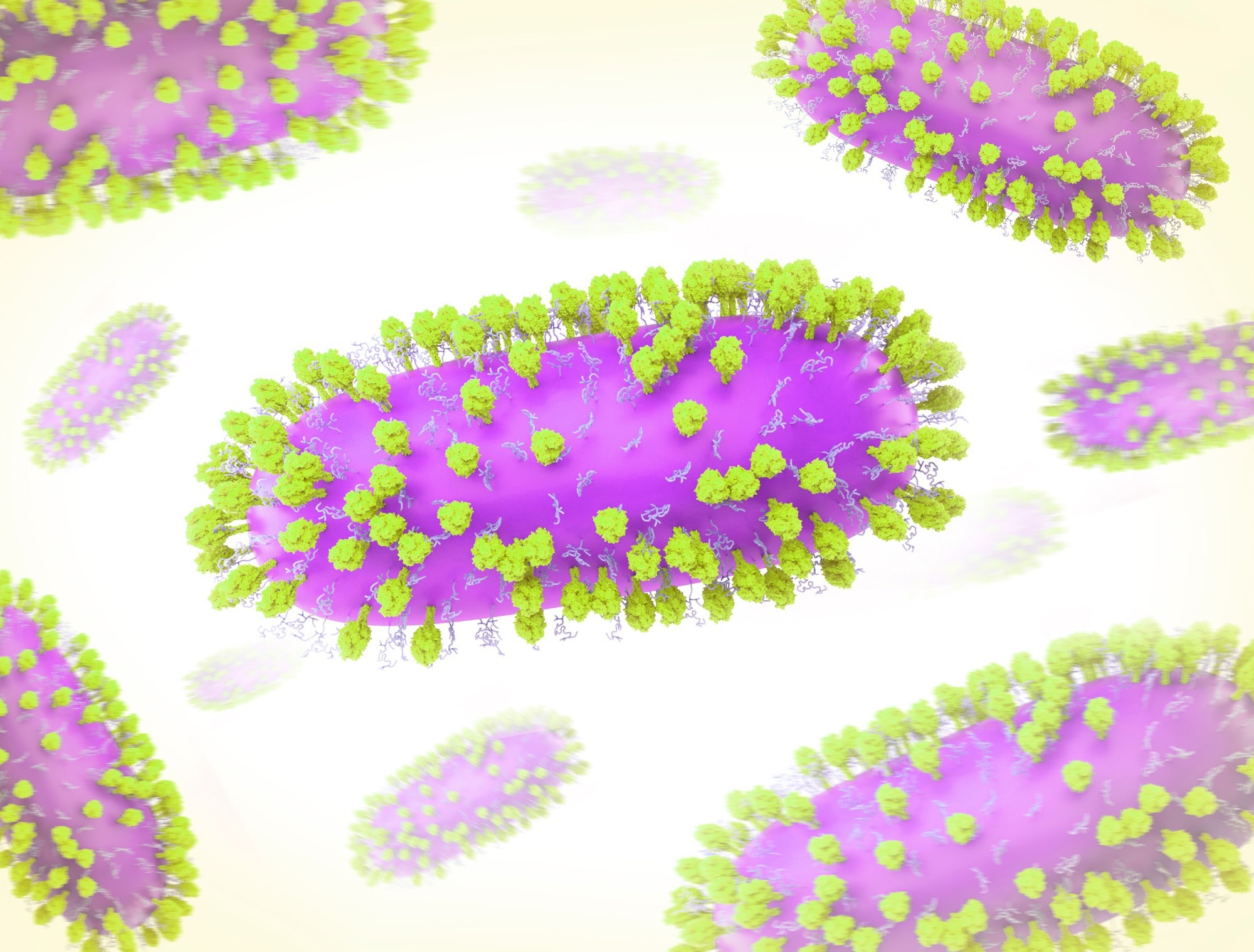
Study: The burden of respiratory syncytial virus in healthy term-born infants in Europe: a prospective birth cohort study. Image Credit: NIAID
About the study
The study involved the enrolment of healthy infants between 1st July 2017 and 31st July 2020 from five different sites representing southern, western, and northern Europe (Netherlands, England, Scotland, Finland, and Spain). All the enrolled children were followed up for at least one year. Parental questionnaires were used to screen for acute respiratory infection (ARI) during the first year of life. In addition, an assessment of all hospital records took place in case of hospitalization for ARI.
During enrolment, the birth cohort participants were invited to be a part of a nested cohort, also referred to as an active surveillance cohort. Each site was recommended to recruit 15 to 20 participants per week to have a cohort with even distribution of months and years of birth. Enrolment in the active surveillance cohort continued until the number of participants reached 200 per site.
Parents were contacted for reported ARI symptoms between 1st October and 1st May. In the case of an ARI, a nasal swab was collected within 72 hours for RSV testing using quantitative reverse transcription PCR (RT-qPCR). Moreover, parents had to complete a diary of healthcare usage and respiratory symptoms for 14 days post the onset of symptoms.
Study findings
The results indicated that a total of 9,154 infants and 993 in the active surveillance cohort were included in the primary analysis. A total of 388 ARI hospitalization was observed, out of which 145 were RSV-positive, 50 occurred during the RSV season but was not tested, and 193 were negative or occurred outside the RSV season. The incidence rate of RSV-associated hospitalization was reported to be 1.8%. It was observed to range between 1.1% in Finland and 2.5% in Spain.
The incidence rate of RSV-associated hospitalization was observed to be higher in children born in autumn compared to those born in winter and spring. The incidence rate was observed to be highest in 2017–18 and lowest in 2019–20. In addition, 84 out of the 145 RSV-associated hospitalizations were reported in children younger than three months. The median duration of hospitalization was reported to be three days and was longer in Spain than in other countries. Moreover, the length of hospitalization was reported to be longer for infants below three months of age.
8 out of 145 RSV-associated hospitalizations required admission to the pediatric intensive care unit, and three required mechanical ventilation. Coinfections with other respiratory viruses were reported in 34 out of 145 RSV-associated hospitalizations, with rhinovirus being the most frequently detected.
The results also reported 1,419 ARI episodes in the active surveillance cohort. 26 out of 1,419 episodes were observed to be positive for RSV. RSV-A was reported in 142 and RSV-B in 111 of RSV-associated ARI. One sample was positive for both subtypes. 131 out of 251 RSV-positive ARI required medical attendance having an incidence rate of 14.1%. The overall incidence rate of RSV-associated ARI overall was observed to be 26.2%. These incidence rates were observed to be highest in Netherlands and lowest in Finland.
Furthermore, wheezing was reported in 87 out of 123 infants admitted with RSV. For the active surveillance cohort, it was reported that 56 out of 118 infants with medically attended RSV-associated ARI and 37 out of 102 infants with non-medically attended RSV-associated ARI.
Therefore, the current study demonstrated a considerable healthcare burden of RSV in healthy term-born infants from Europe. However, since the highest burden occurs during the first year of life, passive immunization and maternal vaccination can play an essential role in reducing the RSV burden.
Limitations
The current study has certain limitations. First, the study did not involve RSV testing in 50 of 388 ARI hospitalizations during the RSV season. Second, information on confection with other respiratory viruses was limited. Third, all countries in Europe were not represented. Fourth, there is a possibility that some ARI episodes were missed. Fifth, the COVID-19 pandemic affected the incidence of RSV in 2020. Finally, the healthcare burden does not highlight the overall burden of RSV.