In a recent study published in the journal Pediatrics, researchers from California evaluated the burden of residual cardiovascular pathology after about six months of treatment for multisystem inflammatory syndrome in children (MIS-C). The tests performed during the follow-up included cardiac magnetic resonance (CMR) imaging, cardiopulmonary exercise testing (CPET), and ambulatory rhythm monitoring. The researchers found that a majority of patients, with or without myocardial injury during hospitalization, showed abnormalities in the cardiac follow-up with a similar prevalence. The findings highlight the need for cardiac follow-up in children with a history of MIS-C treatment.
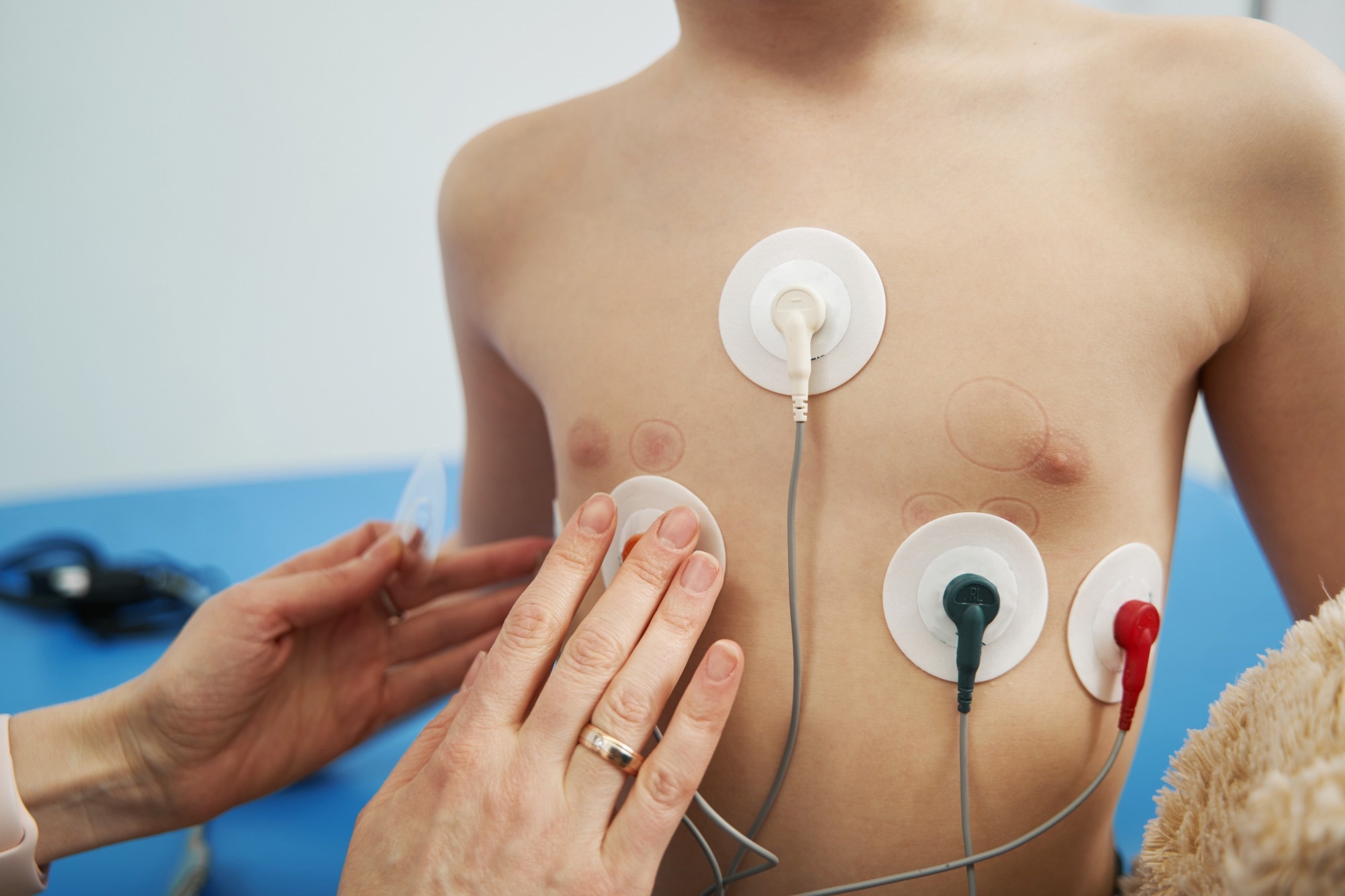
Study: Cardiovascular Follow-up of Patients Treated for MIS-C. Image Credit: Yakobchuk Viacheslav / Shutterstock
Background
MIS-C is a hyperinflammatory response observed in children weeks after infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The condition involves multiple organs, majorly the heart, resulting in several cardiovascular complications. Although complete recovery from MIS-C is possible, the prevalence and severity of cardiovascular issues in the condition are yet to be investigated thoroughly. While evidence suggests that patients with cardiac involvement during acute illness show abnormal findings in cardiac follow-ups, there is a dearth of studies examining the prevalence of abnormal CMR results in patients with and without myocardial injury during MIS-C. Additionally, such patients’ exercise capacity and arrhythmia risk remain to be explored.
Therefore, researchers in the present study assessed the residual cardiac pathology in children using various techniques after a median of 7–8 months of hospitalization due to MIS-C. The results were compared between patients with and without myocardial injury during acute illness.
About the study
A total of 69 patients with at least one cardiac follow-up (at Children’s Hospital Los Angeles) post-MIS-C were included in the study. The mean age of the patients was 10 years, and 64% were male. The patients showed a presence of anti-SARS-CoV-2 serum antibodies. Myocardial injury was defined based on serum troponin levels and echocardiogram findings. Patients’ data were obtained from electronic medical records and inpatient electrocardiograms (ECGs). Two-dimensional echocardiography was performed during the hospital stay and prior to discharge to record the highest coronary artery z-score, worst left ventricular ejection fraction (LVEF), and worst fractional shortening (FS).
Based on clinical indications, patients were followed up about six months post-MIS-C and tested using CMR (n = 47), CPET (n = 57), and ambulatory rhythm monitoring (n = 46). While the CMR was performed using a 1.5 Tesla scanner, the ambulatory rhythm was monitored using a wearable patch monitor. Depending on the patient’s height, CPET was performed using an upright cycle ergometer or treadmill. The statistical analysis included the use of the Shapiro-Wilk test, two-sided Student’s t-test, Wilcoxon rank-sum test, Pearson’s chi-square test, Fisher’s exact test, and the determination of odds ratio.
Results and discussion
Out of the 69 patients studied, 54% showed evidence of myocardial injury during acute illness.
As per the CMR findings, at least one cardiac abnormality was observed in 12 of 26 patients with myocardial injury and in 11 of 21 patients without myocardial injury. The most common abnormalities in CMR were an elevated extracellular volume (ECV, 38%), elevated native T1 (19%), and late gadolinium enhancement (LGE, 13%).
In the ambulatory rhythm monitoring tests, 14% of patients showed intermediate results, a majority of which were in the group with myocardial injury. Four patients out of 33 with myocardial injury showed abnormal findings in the test.
A reduced functional capacity was observed in the CPET results of 82% of patients with myocardial injury and 73% without myocardial injury. The difference in the prevalence of reduced functional capacity, ectopy, or abnormal stress echocardiogram was not found to be statistically significant between the two groups.
Among the 52 patients who underwent at least two tests, 11 showed abnormal findings in both the tests, and one patient showed abnormalities in all the three tests.
Taken together, the results of the study demonstrate the presence of residual cardiovascular pathology in a majority of patients post-MIS-C, warranting a cardiac follow-up in all of them. No significant difference was found in prevalence between patients with myocardial injury during hospitalization and those without. Although the demographic parameters of the studied population indicate the potential generalizability of the findings, the study is limited by its retrospective and single-center design and the lack of patient data on all three modalities.
Conclusion
In conclusion, the findings suggest that cardiac follow-ups are necessary in patients who have recovered from MIS-C, irrespective of the severity of the illness or the presence of myocardial injury during hospitalization. Appropriate cardiac surveillance and counseling could improve the outcomes in these patients, especially those with a risk for premature cardiovascular disease. Longer-term studies are required in the future to understand the persistence and clinical importance of these cardiac abnormalities.